The Economic Aspects of Teledermatology

About the Author
Jim Power is one of Ireland’s leading and best-known economic analysts. Jim has a wealth of experience in delivering insightful economic analysis, forecasts and commentary to both Irish and international audiences. He writes regularly for national newspapers and is a regular contributor to radio and TV debates and discussions, and podcasts such as The Stand and Win Happy. Find out more about Jim Power.
Executive Summary
- Skin cancer is the most common cancer in Ireland, with over 13,000 new cases diagnosed every year. The National Cancer Registry of Ireland (NCRI) expects this number to double by 2040. Melanoma is one of the most serious forms of skin cancer but ‘if spotted early, it is very treatable. If not, it can spread to other parts of the body and cause serious medical issues and ultimately impose considerable additional cost on the health service.
- Waiting lists for dermatology services are long and are not coming down. The outpatient waiting list for dermatology increased by 87.6 per cent between December 2015 and December 2023, from 29,955 to 56,203. In December 2023, adults accounted for 84 per cent of this total at 47,240, and children accounted for 16 per cent at 8,963. In December 2023, there was a further 1,109 patients on the inpatient dermatology waiting list.
- Waiting lists are growing and getting longer. In 2014, 14.9 per cent of outpatients were waiting for more than 12 months; this stood at 19.6 per cent in December 2023. In December 2023, 15.2 per cent of inpatients were on the waiting list for more than 12 months. This deterioration in the length of the waiting list is of deep concern, given that early detection and intervention is essential for a better outcome for the patient and a less expensive treatment process.
- Ireland’s population is growing; it is getting older; and longevity is increasing. These trends have significant implications for the demand for healthcare services. These trends will have significant implications for future incidence of skin cancer.
- Between Census 1961 and Census 2022, the population of Ireland increased by 82.7 per cent from 2.8 million to 5.1 million. In addition to a growing population, the age profile of the population has aged significantly. The population aged 65 years and older has increased by 146.4 per cent from 315,063 to 776,315 over the period from 1961 to 2022.
- The role that teledermatology can play in the diagnosis and treatment of skin cancer in the UK health service is fully recognised in the paper produced by the NHS and British Association of Dermatologists and the systems are in place to support it. The main details are cited in this report.
- Teledermatology is included in the syllabus for dermatology trainees as one of the Fundamentals of Clinical Practice in the UK.
- All Northern Ireland GPs have been issued with a dermatoscope attached to an iPod to take images. This is the only way that referrals will be accepted. This is how the NHS Northern Ireland trusts are dealing with their four-year waiting lists.
- The National Clinical Programme for Dermatology (NCPD) recommended strategic investment in piloting initiatives such as teledermatology and examining the potential for scaling up such initiatives. It concludes that such initiatives, if implemented properly, will shorten waiting lists and times and improve access and quality of care delivery for Irish dermatology patients.
- The main long-term benefit of using teledermatology is to ensure patients receive timely care in the most appropriate setting, thereby increasing capacity for those patients who need face-to-face appointments.
- It is clear that early detection and early intervention is essential for better patient outcomes and also in terms of treatment costs for the health service. The key conclusion of a research article published in the Journal of Public Health relating to Ireland, was that ‘the cost of managing a case of melanoma diagnosed at Stage IV (€122 985) was more than 25 times more expensive than managing a case diagnosed at Stage IA (€4,269).
- Waiting lists for dermatological services are unacceptably high and are proving very persistent. The situation is likely to worsen as demographic and climate-related factors push up the incidence of skin cancer over the coming years. Stakeholders believe the system is in crisis, but that there are proven remedies. The role of teledermatology in reducing waiting lists and achieving better patient outcomes is fully recognised in countries such as the US and UK. The barriers preventing a greater use of these technologies in all Irish hospitals needs to be addressed.
About AllView
AllView Healthcare was founded in 2018. Its technology enables patients, hospitals, and clinics to receive rapid, accurate diagnosis from leading Mohs surgeons, consultant dermatologists and plastic surgeons. Its service works as follows:
- The patient books an appointment.
- The images of the problem area are scanned in nurse led AllView Healthcare clinics.
- A Consultant Dermatologist diagnoses the skin complaint.
- Call from the medical team (GP or registered nurse) with results and treatment plan.
- Results are sent to the patient.
It provides Ireland’s fastest route to access a Consultant Dermatologist diagnosis. In teledermoscopy, a specialist can receive digital dermoscopic lesion images through electronic transmission to examine them. AllView Healthcare is a telediagnostic platform that enables specialists to do this.
Dermoscopy refers to the technical field of utilizing an epiluminescence microscope to view skin lesions in magnification in-vivo. It is especially useful in quickly detecting malignant skin lesions or melanoma. The images and medical notes are assessed remotely by Consultant Dermatologists, without having to see the patient in person or via video link.
About Teledermatology
Telemedicine involves the use of telecommunication technologies to provide medical information and services. The application of the principles of telemedicine to dermatology is referred to as teledermatology.
In effect, teledermatology refers to the use of static digital images to triage, diagnose, monitor, or assess skin conditions without the need for the patient to be physically present. By taking advantage of available technologies, teledermatology can also improve productivity while providing the same level of access to high quality care for the patient.
The main long-term benefit of using teledermatology is to ensure patients receive timely care in the most appropriate setting, thereby increasing capacity for those patients who need face-to-face appointments.
Introduction
Skin cancer is the most common cancer in Ireland, with over 13,000 new cases diagnosed every year. The National Cancer Registry of Ireland (NCRI) expects this number to double by 2040. Melanoma is one of the most serious forms of skin cancer but ‘if spotted early, it is very treatable. If not, it can spread to other parts of the body and cause serious medical issues.’[i]
According to the HSE, when non-melanoma is excluded, melanoma is the fourth most common cancer in Ireland. Around 1,100 new cases of melanoma are diagnosed each year. More than a quarter of skin cancer cases are diagnosed in people under 50, which is early compared to most other types of cancer. Over recent years, skin cancer has become much more common in Ireland. This is thought to be the result of increased exposure to intense sunlight while on holiday abroad. There are approximately 160 deaths every year in Ireland from melanoma.[ii]
Skin cancer is the most common form of cancer in Ireland. There are many different types, but the most common are basal cell carcinoma, squamous cell carcinoma and malignant melanoma. Each year, skin cancer affects approximately 7,000 people for the first time. Medical experts suggest that a large proportion of these will go on to develop a second, third or more skin cancers. Once a patient has had one type of skin cancer, they are at a higher risk of developing other forms of the disease. Most skin cancers are not life-threatening, with even the most dangerous form, malignant melanoma curable if caught in the early stages.[iii]
Against a background of an ageing population, more foreign travel, and climate change, the expectation is that skin cancers will become more common in Ireland over the coming years.
This paper is not a medical paper written by a medical specialist, but rather it is a paper written by an economist examining the economic effects of skin cancer and the pressure it is putting on the health service.
The facts are clear, even to a non-medical person. Waiting lists for dermatology are very high and growing. If caught in time, most forms of skin cancer can be cured, but the obvious risk it that because of the long waiting lists, the cancer will have advanced by the time a dermatologist gets to examine it and may be very difficult to cure. The more advanced skin cancer is, the more difficult it will be to treat, and it will prove considerably more expensive for the healthcare service.
This report was commissioned by AllView Healthcare. It is based on an objective analysis of the use of teledermatology to help diagnose skin cancers at an early stage. It seems clear that the use of this technology has the potential to reduce waiting lists for dermatology services, thereby ensuring that those who need treatment the most get it as fast as possible; it can reduce the costs of treatment to the health service; and most importantly it can help ensure a better health outcome for the patient.
The paper was completed using a combination of desk-based research; international experience; and interviews with key stakeholders with expertise in dermatology.
The paper is structured as follows:
- Analysis of the trends in waiting lists for dermatology services in Ireland.
- Demographic trends in Ireland.
- An explanation of teledermatology and an assessment of the role it can play in detecting skin cancers.
- Research findings from health research.
- The UK as an example of a health service that has embraced teledermatology.
The economic and financial benefits for the Irish health service from embracing teledermatology.
Dermatology Waiting Lists in Ireland
The trend in the outpatient dermatology waiting list has increased rapidly since December 2015. The outpatient waiting list increased by 87.6 per cent between December 2015 and December 2023, from 29,955 to 56,203. In December 2023, Adults accounted for 84 per cent of this total at 47,240, and children accounted for 16 per cent at 8,963.
In December 2023, there was a further 1,109 patients on the inpatient dermatology waiting list.
Table 1 shows the waiting list period for dermatology. In 2014, 14.9 per cent of patients were waiting for more than 12 months; this stood at 19.6 per cent at the end of 2023. 15.2 per cent of dermatology inpatients were waiting more than 12 months. This deterioration in the length of the waiting list is of deep concern, given that early detection and intervention is essential for a better outcome and a less expensive treatment process.
| Dec-14 | May-23 | |||
| Total | % | Total | % | |
| 0-6 Months | 18,972 | 58.8% | 31,371 | 55.8% |
| 6-12 Months | 8,480 | 26.3% | 13,816 | 24.6% |
| 12-18 Months | 3,534 | 10.9% | 4,469 | 8.0% |
| 18+ Months | 1,298 | 4.0% | 6,547 | 11.6% |
| Total | 32,284 | 100.0% | 56,203 | 100.0% |
Table 1: Outpatient Waiting List Period for Dermatology
Demographic Change in Ireland & Skin Cancer
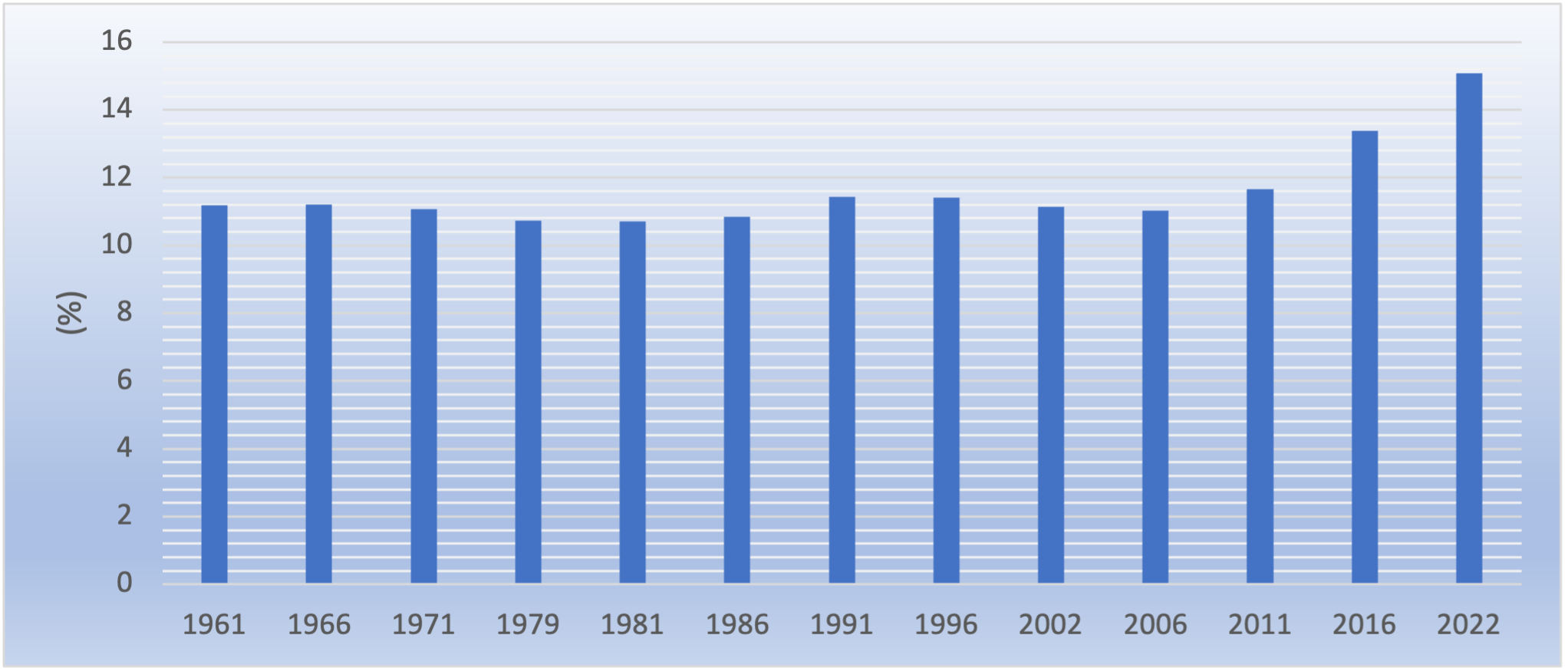
Between Census 1961 and Census 2022, the population of Ireland increased by 82.7 per cent from 2.8 million to 5.1 million. In addition to a growing population, the age profile of the population has aged significantly. The population aged 65 years and older has increased by 146.4 per cent from 315,063 to 776,315.
As a percentage of the total population, the over 65 age cohort has increased from 10.7 per cent in 1981 to 15.1 per cent in 2022. OECD data[iv] suggest that in 2023, life expectancy stood at 82.4 years. Life expectancy for males stood at 80.8 years for males and 84.4 years for females.
Ireland’s population is growing; it is getting older; and longevity is increasing. These trends have significant implications for the demand for healthcare services. In the context of the subject matter of this paper, these trends will have significant implications for future incidence of skin cancer.
| TYPE OF SKIN CANCER | <50 YEARS | 50-59 YEARS | 60-69 YEARS | 70-79 YEARS | >80 YEARS |
| Malignant Melanoma (MM) – Male | 20% | 16% | 24% | 24% | 16% |
| Malignant Melanoma (MM) – Female | 31% | 17% | 19% | 17% | 16% |
| Basal Cell (BC) – Male | 12% | 15% | 27% | 31% | 15% |
| Basal Cell (BC)- Female | 15% | 16% | 24% | 26% | 19% |
| Squamous Cell Carcinoma (SCC) – Male | 3% | 8% | 20% | 38% | 31% |
| Squamous Cell Carcinoma (SCC) – Female | 3% | 7% | 16% | 30% | 44% |
Table 2: Age Distribution of Skin Cancer 2011-2015
Source: National Cancer Registry, Cancer Trends, July 2017
Data from the National Cancer Registry[v] show that like many cancers, skin cancers are more common in older age.
Between 2011 and 2015:
- 40 per cent of MM cancers in males were in patients aged over 70 years.
- 33 per cent of MM cancers in females were in patients aged over 70 years.
- 46 per cent of BC cancers in males were in patients aged over 70 years.
- 45 per cent of BC cancers in females were in patients aged over 70 years.
- 69 per cent of SCC cancers in males were in patients aged over 70 years.
- 74 per cent of SCC cancers in females were in patients aged over 70 years.
With Ireland’s ageing population, it seems clear that the incidence of the various forms of skin cancer will increase significantly over the coming years and put intolerable pressure on a dermatology service that is characterised by growing and lengthening waiting lists.
Research Findings
Picking up patients with skin cancer early is essential and will provide better health outcomes for the patient and will significantly reduce the cost of treatment to the health service. This section cites some of the international evidence in support of teledermatology in achieving better outcomes for the patient and the health service.
A US research paper conducted a retrospective study of 59,279 primary care patients presenting with a skin lesion from January through to June 2017.[vi] This study demonstrated the effectiveness of asynchronous store and forward teledermatology, which is more effective than synchronous teledermatology. The quality of the images is much superior.
The authors began by stating that the effectiveness and value of teledermatology and face-to-face workflows for diagnosing lesions are not adequately understood. The study compared the risks of biopsy and cancer diagnosis among two face-to-face workflows (direct referral and roving dermatologist) and 4 teledermatology workflows.
One teledermatology workflow achieved high-resolution images with use of a dermatoscope-fitted digital camera, a picture archiving and communication system, and image retrieval to a large computer monitor (in contrast to a smartphone screen). Compared with direct referral, this workflow was associated with a 9 per cent greater probability of cancer detection, a 4 per cent lower probability of biopsy, and 39 per cent fewer face-to-face visits. Other workflows were seen to be less effective.
US insurance and Medicare in the states reimburse for teledermatology, demonstrating that it is recognised as standard of care in the US also.
A UK study pointed out that there is a paucity of published evidence of established teledermatology (TD) services in the UK. An in-house TD service using store-and-forward technology was set up at a large regional dermatology department in 2004. Retrospective data were retrieved using the electronic patient database, from 31st July 2004 to 31st July 2018. More detailed information on patient outcomes was obtained from patient notes and histology records. A paper questionnaire was distributed to 100 patients to obtain patient feedback.
This research showed that in total, 40 201 teleconsultations were made over 14 years, and 64 per cent of cases were coded, of which 77 per cent were lesions. The most common coded lesions were benign naevus (25 per cent), seborrhoeic keratosis (22 per cent) and basal cell carcinoma (19 per cent). Of the total number of cases, 50 per cent were discharged to their general practitioner with advice, 34 per cent were booked for surgery and 16 per cent were booked for a face-to-face appointment. In the survey, 82 per cent of patients surveyed felt that the service was ‘good’ or ‘very good’. A detailed study between 1 January 2015 and 1 January 2016 showed that there were 383 patients (10 per cent) with no diagnosis made following teleconsultation, suggesting diagnostic uncertainty. Reasons for this included lack of diagnostic features, possibility of malignancy and service factors. Within this cohort, there was 68 per cent diagnostic concordance.
This study that the setting up of the successful TD service at a UK centre, has prevented 16 282 face-to-face appointments over 14 years. Patient feedback has been very good. Review of cases with diagnostic uncertainty provides important information for service improvement and has not previously been documented.[vii]
One of the arguments cited against the role of teledermatology is that the patient doesn’t get a full skin examination. Many centres in Ireland do not conduct a full skin examination. The reality is that at the teledermatology appointment if the patient has many moles they are brought in for full skin examination or if they have other risk factors such as being immunosuppressed or have a history of previous skin cancers. Patients have up to five lesions imaged at the appointment.
A research publication from Cork showed that in over 700 patients with full skin examinations no incidental finding of melanoma was detected. This research concluded that ‘full skin examination (FSE) may improve the detection of malignant melanoma (MM). The objective of this study was to assess the safety of targeted lesion examination (TLE) compared to FSE in our pigmented lesion clinic (PLC). Patients attending PLC were randomised in a 2:1 ratio to FSE (intervention) or TLE (standard care). Demographic details and risk factors were documented. FSE and TLE were timed. Of 763 participants, 520 were assigned to FSE and 243 were assigned to TLE. On average, FSE took 4.02 minutes and TLE took 30 seconds. Thirty‐seven (7.1%) patients had incidental findings on FSE. Twelve patients (2.3%) had additional lesions biopsied. No additional melanomas were detected that would have been missed by use of the standard protocol. This study suggests that in low‐risk patients attending a PLC referred with a lesion of concern, the possibility of missing incidental cutaneous malignancies using lesion‐directed examination is low.’[viii]
Teledermatology in The UK Health Service
NHS And British Association of Dermatologists
A paper written by the NHS and the British Association of Dermatologists in April 2022[ix] advised that targeted interventions are needed to help recover from the COVID-19 pandemic, particularly in relation to the early diagnosis of melanoma, as well as to manage the increase in demand from those who were reticent about coming forward during the pandemic.
The context for the guidance in the paper is laid out clearly. Skin cancer is the most common cancer in the UK and dermatology services receive more urgent referrals for suspected cancer than any other specialty. Approximately 50 per cent of the one million dermatology referrals are suspected skin cancer two week wait referrals. The number of patients diagnosed with melanoma and squamous cell carcinoma is approximately 6 per cent of all two-week wait skin referrals. It is recognised that a significant proportion of patients are seen with non-relevant skin lesions. Prior to the COVID-19 pandemic, the requirement was that all patients have face-to-face appointments in specialist dermatology departments. The ageing population is expected to put further pressure on the specialty, as skin cancer occurs much more frequently in the elderly and can be more difficult to treat in the presence of age-associated co-morbidities.
The paper issued guidance on new models of service delivery for systems to consider as they seek to optimise suspected two-week wait skin cancer referrals both to tackle the backlog and to meet new demand as services are restored by: It suggests:
- Harnessing new technology, in particular teledermatology and digital referral platforms to reduce unnecessary hospital attendances.
- Developing ‘spot clinics’ – these allow consultant-led dermatology teams to review a large group of suspected skin cancer two-week wait referrals in a community or hospital setting.
The paper points out that the traditional pathway for skin cancer two-week wait referrals requires all patients to attend a secondary care dermatology department for a face-to-face appointment. This model will continue to be available where other clinical pathways are unsuitable or unavailable. It is recognised that this pathway is particularly well suited to patients with multiple suspicious lesions, a history of skin cancer and other risk factors.
However, to manage suspected skin cancer two-week wait referrals in a more streamlined way, it is recommended that systems should consider adopting a range of different services to meet local need. These can supplement the traditional face-to-face model by enabling systems to adapt solutions to local circumstances. It believes that the use of teledermatology for a new virtual pathway will significantly reduce the need for patients to attend hospital.
Teledermatology referral refers to the use of asynchronous store and forward teledermatology, where high quality images accompany the two-week wait dermatology referral to enable consultant triage, ensuring face-to-face hospital attendance only when necessary.
It is pointed out that a virtual teledermatology two-week wait pathway requires:
- High quality macroscopic and dermoscopic images as these are the ‘reasonable diagnostics’ needed to exclude cancer.
- A triage outcome that permits the specialist clinician to request to see the patient face to face if required.
- The facility to communicate directly with the patient and their GP.
Outcomes from the virtual teledermatology two-week wait referral that ‘stop the clock’ on the referral can include:
- The patient has an interaction with a consultant or a member of their team (via telephone, video or face-to-face consultation).
- The patient is booked directly for surgery and receives appropriate pre-operative advice and counselling.
Different models for high quality image capture will be required to support this model and will need to be locally agreed. These could include:
- Images taken by a suitably trained healthcare professional in a GP surgery.
- Images taken by suitably trained healthcare professionals (for example, community nurses or medical photographers) in a community hub or secondary care setting.
UK Syllabus For Dermatology Trainees
Teledermatology is in the syllabus for Dermatology trainees as one of the Fundamentals of Clinical Practice in the UK.[x] The syllabus document was produced by the British Association of Dermatologists (BAD) Education Subcommittee, in conjunction with the Joint Royal College of Physicians Training Board (JRCPTB) Dermatology Specialist Advisory Committee (SAC).
The Syllabus Guidance is intended to be used as a supporting document for the GMC 2021 Dermatology Curriculum. It provides detailed competencies to support the high-level Capabilities in Practice (CiPs) outlined in the curriculum. To be able to carry out safe and effective teledermatology consultations with General Practitioners or other Health Care Professionals in Primary, Intermediate or Secondary care the following areas are included in the syllabus covering knowledge requirements, skills requirements and teaching and learning methods:
Knowledge
- Demonstrate awareness of the potential benefits and risks of teledermatology in comparison to face-to-face consultation for inflammatory diseases.
- Demonstrate awareness of the potential benefits and risks of teledermatology in comparison to face-to-face consultation for skin cancer and lesions.
- Describe the role of teledermatology for patient triage from primary to secondary care.
- Describe the role of teledermatology for skin cancer diagnosis and management.
- Discuss the role of teledermatology in patient management within secondary care, including on-call advice and inter-specialty referral.
- Describe the benefits and limitations of different mobile devices for teledermatology delivery. Describe the main principles involved in obtaining high quality medical images.
- Demonstrate awareness of the medicolegal issues relating to consent, storage and transfer of patient images.
- Demonstrate awareness of Information Technology and governance policy regarding teledermatology.
- Demonstrate awareness of the range of teledermatology referral pathways used across the NHS Describe the principles of audit for evaluation of teledermatology services.
Skills
- Demonstrate the ability to take a high-quality medical image (localizing and close-up) using a mobile device.
- Demonstrate the ability to take a high quality dermoscopic image using a mobile device.
- Demonstrate secure transfer and storage of a medical image taken with a mobile device.
- Provide a safe and comprehensive teledermatology consultation for a patient with a rash.
- Provide a safe and comprehensive teledermatology consultation for a patient with suspected skin cancer.
Teaching and Learning Methods
- Observation of photography skills.
- Observation of teledermatology reporting skills.
- Participation in teledermatology reporting service.
- Online resources including e-learning for Health e-Dermatology modules.
- Assessment of understanding of national guidelines for teledermatology and mobile devices. Methods agreed by Educational Supervisor and Trainee
Conclusion
The role that teledermatology can play in the diagnosis and treatment of skin cancer in the UK health service is fully recognised in the paper produced by the NHS and British Association of Dermatologists and the systems are in place to support it. Teledermatology is also included in the syllabus for dermatology trainees as one of the Fundamentals of Clinical Practice in the UK.
All Northern Ireland GPs have been issued with a dermatoscope attached to an ipad to take images. This is the only way that referrals will be accepted. This is how the NHS Northern Ireland trusts are dealing with their four-year waiting lists.
The Patient And Financial Benefits of Early Diagnosis
Access to care in an appropriate timeframe is essential for patients with a skin condition. Picking up patients with skin cancer early is essential and can generally be life saving for patients.
The dermatology system in Ireland currently works on the basis of a patient with a skin condition getting a letter of referral from the GP to a specialist, but they typically have to wait weeks, months or even years for an appointment. This means that patients with skin cancer will be at a much more advanced stage and the chances of survival will be reduced and the cost of treatment will be significantly higher.
The reality is that many patients who present to dermatology specialists do not need to be seen, but it is difficult to triage patients. Teledermatology does provide a solution. It acts as a screening mechanism and ensures that patients with a problem are diagnosed quickly and treated quickly.
A 2012 study highlights clearly the issues involved.[xi] Faruk et al conclude that metastatic melanoma (MM) is a fatal disease with a rapid systemic dissemination. This study was conducted to investigate the metastatic behaviour, timing, patterns, survival, and influencing factors in MM. 214 patients with MM were evaluated retrospectively. Distant metastases (82 per cent) were the most frequent for patients initially metastatic. The median and 1-year survival rates of initially MM patients were 10 months and 41 per cent, respectively. The median time to metastasis for patients with localized disease was 28 months. The timing of appearance of metastases varied minimally; however, times to metastases for distant organs varied greatly. Crucially, the research found that the median time to development of second metastases from the time of first metastases was 11 months. The timing of appearance of metastases according to metastatic M1 stage varied greatly. Thus, the median times to development were 20 and 21 months for M1A and M1B, respectively, and M1C had highly lower times (9 months).
The study showed that the median and 1-year survival rates of all patients were 12 months and 49 per cent, respectively. Outcome was higher in M1A than visceral metastases. The research concluded, ‘the fact that over half of all recurrences/metastases occurred within 3 years urges us to concentrate follow-up in the early time periods following diagnosis. Because the clinical behaviour of MM is variable, the factors for survival consisting of site and number of metastases should be emphasized.’
Early detection and early intervention are essential for better patient outcomes and also in terms of treatment costs for the health service. One study published in the Journal of Public Health (https://doi.org/10.1093/pubmed/fdac154)[xii] examined the melanoma-related costs by disease stage and phase of management in Ireland. The conclusions are stark.
The research was based on a detailed decision model, describing the melanoma care pathway by disease stage from diagnosis, through treatment and follow-up over a 5-year time frame from the perspective of the Irish healthcare system. The model was populated with real-world data from the National Cancer Registry Ireland. The key conclusion was that ‘the cost of managing a case of melanoma diagnosed at Stage IV (€122 985) was more than 25 times more expensive than managing a case diagnosed at Stage IA (€4,269). Total costs were sensitive to the choice of immunotherapeutic and targeted drug, duration of treatment and proportion of patients receiving immunotherapy agents.’
The authors advised that the rising incidence of melanoma and high cost of new novel therapies presents an immediate challenge to cancer control and public health globally and that the study highlights the vastly different costs involved in the treatment of cancers detected at an early or late stage in its progression, and the potential return on investment for prevention versus high-cost treatment.
The longer a skin cancer is left untreated the, the thicker it will get and the more difficult to cure.
The Breslow Depth is a helpful measure of how far melanoma has invaded the body. Knowing the depth of melanoma is helpful because it is important when considering future treatment. Breslow Depth is the measurement of the depth of the melanoma from the surface of the skin down through to the deepest point of the tumour. It is measured in millimetres (mm) with a small ruler, called a micrometer. The thinner the depth of the cancer, the less expensive the care, as the surgery tends to be minor rather than invasive. Apart from cost, this is better for the recovery of the patient.
The Clark Level is a staging system that describes the depth of melanoma as it grows in the skin. The doctor may give the patient a level for the melanoma in addition to or in place of a stage. These designations are not interchangeable.
The Clark Scale has five levels:
- Level 1: Melanoma is confined to the epidermis (the outer layer of the skin).
- Level 2: Melanoma has invaded the papillary dermis (the outermost layer of the dermis, the next layer of skin).
- Level 3: Melanoma has invaded throughout the papillary dermis and is touching on the next, deeper layer of the dermis.
- Level 4: Melanoma has invaded this next deeper layer, the reticular dermis.
- Level 5: Melanoma has now invaded the fat under the dermis.
The current staging system adopted by the American Joint Committee on Cancer (AJCC) no longer considers the Clark Level. This is because the Clark level has been found to be less prognostic and more subjective than other alternatives. The AJCC system assigns a stage based on tumor, node, metastasis (TNM). The goal is that melanomas of the same stage will have similar characteristics, treatment options, and outcomes.[xiii]
Conclusions
Access to see a dermatologist as quickly as possible is essential, because if caught early, many skin conditions can be cured. This is vital for the patient outcome, but also for the cost involved for the healthcare system.
Some stakeholders believe that potentially fatal skin cancers are being missed or treatment delayed due to the slow uptake of a private teledermatology service under contract to the HSE to clear waiting lists. One hospital which signed up said that one in five patients it referred were diagnosed with skin cancer, including some with malignant melanomas.
AllView Healthcare has received patients from just five hospitals in Dublin, Drogheda, and Cavan since winning a HSE contract in October 2021, out of 27 offering various levels of adult dermatology care. It is suggested this may be partly down to a dispute between consultants. AllView Healthcare claims it has the capacity to take on an extra 19,000 patients that went unused and it is looking like the same capacity for 2023 will go unused unless more hospitals open their doors. Hospitals using AllView Healthcare have achieved the largest waiting-list reductions. One dermatology consultant suggested that ‘one in five people of those cases we sent to AllView Healthcare had a skin cancer. On average their care was brought forward by 14 months‘.
The National Clinical Programme for Dermatology (NCPD)[xiv] gave recognition to a pilot study for the use and benefits of teledermatology in an Irish context. It states that ‘the use of photography as a triage tool offers the potential to shorten waiting lists and improve healthcare access and delivery, while identifying and fast-tracking patients with suspicious skin lesions. The process will also allow patients with evidently benign lesions to be discharged, representing cost efficiencies for dermatology.’
The NCPD recommended strategic investment in piloting initiatives such as teledermatology and examining the potential for scaling up such initiatives. It concludes that such initiatives, if implemented properly, will shorten waiting lists and times and improve access and quality of care delivery for Irish dermatology patients.
Waiting lists for dermatological services are unacceptably high and are proving very persistent. The situation is likely to worsen as demographic and climate-related factors push up the incidence of skin cancer over the coming years. Stakeholders believe the system is in crisis, but that there are proven remedies. The role of teledermatology in reducing waiting lists and achieving better patient outcomes is fully recognised in countries such as the US and UK. The barriers preventing a greater use of these technologies in all Irish hospitals needs to be addressed.
References
[i] Irish Cancer Society
[ii] www.hse.ie, Overview-Skin cancer (melanoma)
[iii] stjames.ie/cancer/typesofcancer/skincancer
[iv] OECD Health at a Glance 2023 Country Note Ireland.
[v] National Cancer Registry, Cancer Trends, July 2017
[vi] jaad.org/article/S0190-9622(19)30178-1/pdf
[vii] Mehrtens SH, Shall L, Halpern SM. A 14-year review of a UK teledermatology service: experience of over 40 000 teleconsultations. Clin Exp Dermatol. 2019 Dec;44(8):874-881. doi: 10.1111/ced.13928. Epub 2019 Feb 14. PMID: 30767255.
[viii] researchgate.net/publication/349670775_Bare_necessities_The_utility_of_full_skin_examination_in_the_COVID19_era
[ix] cdn.bad.org.uk/uploads/2022/07/29094510/B0829-Suspected-skin-cancer-two-week-wait-pathway-optimisation-guidance.pdf
[x] Dermatology Syllabus Guidance August 2021. British College of Dermatology, British Association of Dermatology, Joint Royal Colleges of Physicians Training Board.
[xi] Faruk Tas, “Metastatic Behaviour in Melanoma: Timing, Pattern, Survival, and Influencing Factors”, Journal of Oncology, vol. 2012, Article ID 647684, 9 pages, 2012. doi.org/10.1155/2012/647684
[xii] Melanoma-related costs by disease stage and phase of management in Ireland Grainne E. Crealey, Caitriona Hackett, Katharine Harkin, Patricia Heckmann, Fergal Kelleher, Áine Lyng, Triona McCarthy, Maria McEnery, Clare Meaney, Darren Roche, Anne-Marie Tobin.
[xiii] Breslow Depth and Clark Level curemelanoma.org
[xiv] hse.ie/eng/about/who/cspd/ncps/dermatology/resources/national-clinical-programme-for-dermatology-a-model-of-care-for-ireland.pdf